"Pain is a signal that your arthritis is active, and we don't want to just treat the pain, we want to treat the problem." Psoriatic arthritis is a type of inflammatory arthritis that can occur in people who have psoriasis. It can include anything from arthritis of the small joints of the hands to inflammatory arthritis of the spine to Achilles tendinitis.
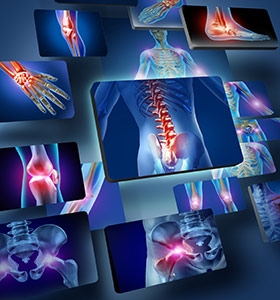
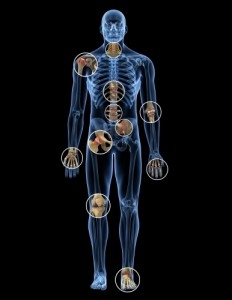
Psoriatic arthritis is a type of inflammatory arthritis that can occur in people who have psoriasis. It can include anything from arthritis of the small joints of the hands to inflammatory arthritis of the spine to Achilles tendinitis. About 30% of people with psoriasis will develop psoriatic arthritis, and it usually appears 5 to 10 years after the psoriasis begins. A small percentage (10%) of people with psoriatic arthritis will develop it before they develop the skin condition of psoriasis.
How will I know if I am developing psoriatic arthritis?
If you have psoriasis and you get any sort of joint symptoms that last more than a few weeks, you should be evaluated to see if you have developed psoriatic arthritis. The primary symptoms are pain and stiffness in a joint or joints. One of the hallmarks is morning stiffness, where it may take you 45 minutes or more to feel loosened up. Tendinitis is another symptom. Interestingly, there isn't a good correlation between the severity of someone's psoriasis and the severity of the arthritis they develop. People with mild psoriasis might be just as likely to develop arthritis as someone with a severe form of the skin disease. Everyone should be aware of that.
What kind of a doctor should I see?
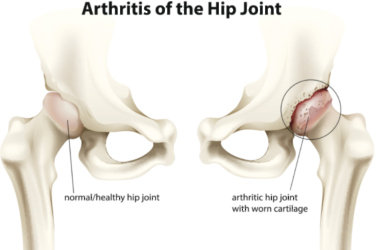
If you think you could have psoriatic arthritis, you should go to a rheumatologist. Many people who have psoriasis are treated by a dermatologist, and that's a good place to start. But they are not as adept at evaluating joint problems. The key is recognizing whether the arthritis is inflammatory or degenerative, such as osteoarthritis, and a lot of dermatologists and primary care physicians won't necessarily be able to tell.
Without treatment, will psoriatic arthritis cripple the joints like rheumatoid arthritis can?
It probably causes damage to joints in a smaller percentage of people than rheumatoid arthritis. It's fair to say that 80% to 90% of people with rheumatoid arthritis will have ongoing damage to joints without good treatment, but that number is probably closer to 40% in people with psoriatic arthritis.
What's the first treatment I will probably be prescribed?
The first treatment you'll be Nonsteroidal anti-inflammatory drugs (NSAIDs) like naproxen, ibuprofen, and diclofenac. But it depends on the patient. First I do a more thorough evaluation of what's going on. If X-rays already show evidence of joint damage, it's appropriate to step it up right from the beginning and consider methotrexate or other systemic drugs. On the other hand, if there is no sign of damage and the symptoms are relatively mild, I would start with NSAIDs. We don't treat everybody aggressively out of the gate, because we would end up treating some people who may not need it. We don't have the best prognostic clues yet to say who is going to develop more damage, but there is a big effort among researchers to try and derive them.
Are the new biologics good for treating psoriatic arthritis?
They are very effective. They have typically been used after methotrexate, but for a variety of reasons, doctors will sometimes use them before. Methotrexate tends not to be as effective at treating psoriatic arthritis as it is at treating rheumatoid arthritis, and because of the side effects, some doctors may start out with the biologics. But there is no clear standard of care at this point. You have to remember that this disease affects both joints and skin, so what is happening in both often drives what you do. A patient with bad skin disease whose joint disease is not that bad might still consider a biologic. If you can treat the skin with topical medications and light therapy, but the joint disease is bad, I might proceed to a systemic like methotrexate, or a biologic. It's critical to consider both as you make treatment decisions.
What side effects do you need to worry about with the medications that treat psoriatic arthritis?
With methotrexate, the concern has always been liver damage—scarring and cirrhosis. We know that monitoring closely can help identify early signs of that before it gets bad. There is some uncertainty as to whether people with psoriasis and psoriatic arthritis might be more susceptible to liver disease, but it has not been sorted out. We worry about blood counts, because the drug can affect bone marrow. So we monitor that closely. Both methotrexate and biologics target the immune system, so there is a significant concern about infections. Common bacterial infections, such as pneumonia or sinusitis, as well as less common infections, such as tuberculosis and fungal infections, can occur more frequently. We have to be attuned to those.
With methotrexate, regular laboratory monitoring is important. With biologics there are no specific guidelines for testing. But usually a physician will follow you closely and make sure things are going well. These are not drugs where we say, "OK, here's a prescription for the next year." We like to see people at a minimum of every three to four months. We want to be on top of it if something goes wrong.
How can I minimize pain at home?
There is nothing specific for everybody. Some people find that heat can be helpful, but I would steer people away from focusing on just treating the pain. Pain is a signal that your arthritis is active, and we don't want to just treat the pain, we want to treat the problem.
If I am in pain, should I go back to my doctor?
Yes, because the pain suggests that the disease is not controlled, and that may translate to more problems in the long term. We don't want to let that happen.
Source: health.com